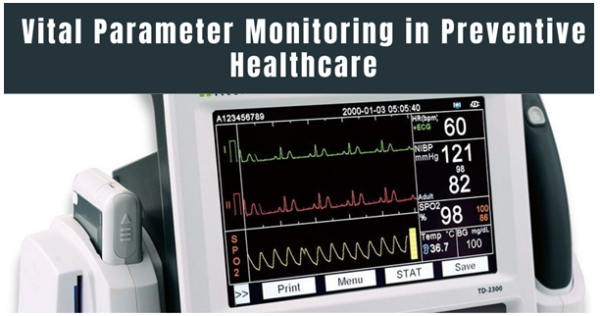
The field of healthcare is experiencing a profound alteration, instable from a responsive model where treatment is started only after a disease establishes to a proactive, patient-centric approach. Such evolution is enhanced by technical progress that allows constant and real-time health monitoring. At the heart of this paradigm move is dynamic parameter monitoring, the regular measurement of a patient’s vital physiological functions such as heart rate, blood pressure, respiratory rate, and body temperature. Such technology is becoming a keystone of modern medicine which extending beyond the hospital setting into the home and normal life through wearable devices and remote patient monitoring systems.
The rising position of this technology is emphasised by the rising global burden of chronic diseases. For instance, Pristine Market Insights stated that the number of individuals affected by ischemic heart disease is possible to rise to 1845 out of every 100,000 people by 2030. Such an offensive statistic highlights the urgent need for advanced solutions to prevent and manage such conditions.
The vital parameter monitoring is crucial for both preventive and projecting healthcare. The constant tracking of an individual’s vital signs permits the primary recognition of delicate changes or irregularities that may indicate the onset of a health issue, permitting for timely intervention and avoiding severe health crises. Such ability is a main driver for the growth of the vital parameter monitoring market as it delivers an influential tool for anticipating future health events and moving healthcare from simply treating illness to actively keeping wellness.
Preventive Healthcare and Vital Monitoring
The protective healthcare is a practical approach to medicine that takes efforts to prevent diseases and injuries before they occur, rather than treating them after they’ve advanced. The main purpose is to save a patient’s well-being and decrease their risk of infection. It is completed through actions such as vaccinations, regular treatment. Recognising risk landscapes and early signs of disease and taking protective care can lead to improved long-term health outcomes and lower healthcare costs.
- Role of Vital Monitoring in Prevention
Continuous monitoring of critical parameters is a serious means of preventive health care. With vital monitoring, instead of a periodic measurement in a doctor’s office, people have considerable information in real-time about various important physiologic measures like heart rate or blood pressure that is usually obtained through wearable devices. Continuous monitoring allows the user to detect small changes or deviations that might be symptomatic of a health issue. By giving an example, if someone’s blood pressure is showing consistent and progressive increases each week or month, they will be cautioned that they are experiencing developing hypertension. In some people, an inconsistency in heart rhythm or an increased resting heart rate may be an indicator of emerging cardiovascular issues. Early warning systems like those provide an opportunity for various interventions and lifestyle changes and medication changes, which can prevent fitness-related problems from progressing to disease.
- Real-World Applications
The use of vital parameter monitoring in preventative health care is already having a significant impact. In terms of hypertension prevention, wearable blood pressure monitors and smartwatch apps can annually monitor relevant daily changes and warn users when readings consistently indicate higher than the normal range. Such data can be provided to the user’s physician, who may advise lifestyle changes such as less salt and more activity, as well as stress management that is before a diagnosis of high blood pressure.
Continuous glucose monitoring devices have altered the game for diabetes supervision. Not a “vital parameter” in the generally understood sense, they are still vital for preventing complications in susceptible individuals. With CGMs, the users accept real-time blood glucose analyses and can study the effect of diet and exercise on blood sugar levels. This is supportive for the user and also for the health care provider to use data to make tailored interventions that keep glucose within normal range. This prevents the transition of prediabetes to type 2 diabetes and mitigates severe complications for already diagnosed individuals.
Benefits of Vital Parameter Monitoring in Healthcare
The benefits of vital signs monitoring are many and varied, resulting in a shift in the way healthcare and health delivery systems are being thought of and conducted. Whole body monitoring gives healthcare providers the ability to recognise small changes in a patient’s vital signs that may go unnoticed by sporadic spot-checks. Continuous monitoring with alarmed surveillance gives proactive response elements where a healthcare provider could potentially be informed and be able to step in to provide timely intervention, and recognise there is a problem that needs attention.
For example, recognising early precursors to an impending event. There is definitely a benefit of reducing hospital admissions and readmissions for expensive acute care treatment for everyone, including health systems and individual patients, by dealing with the pre-symptomatic issue. Such a method suggestively recovers patient outcomes, mainly for those organisations’ chronic conditions such as heart failure or hypertension. Constant data streams offer a more complete picture of a patient’s health, which permits doctors to fine-tune treatment plans with superior precision.
The Future of Vital Parameter Monitoring in Healthcare:
- Advancements in Technology
The upcoming of vital parameter monitoring is being shaped by cutting-edge technologies. AI and machine learning will analyse huge datasets from wearables to recognise subtle, analytical health patterns. Meanwhile, 5G networks and IoT devices will protection unified, real-time data transmission with low latency, which enhances the speed and consistency of inaccessible monitoring.
- Integration with Telemedicine
The vital monitoring will become extremely integrated with telemedicine platforms. Such interaction will allow doctors to conduct virtual consultations with an inclusive, real-time view of a patient’s health data. Such a thing allows for more informed remote diagnoses, personalised advice, and rapid interventions without the need for in-person visits.
- Personalized Healthcare
The continuous dynamic sign data will be the foundation of accurately personalised healthcare. Analysing an individual’s exclusive physiological trends and baselines, doctors can move beyond one-size-fits-all treatments. Such data will allow for customised care plans, proactive routine approvals, and drug dosages exactly tailored to a patient’s specific requirements.
Conclusion:
The vital parameter monitoring is key for the future of healthcare, altering it from a reactive to a proactive system. By allowing early detection, improving chronic disease management, and decreasing costs, it is the keystone of defensive and projecting medicine. Continual investment in these technologies is important to make a more efficient and personalised healthcare landscape for all.